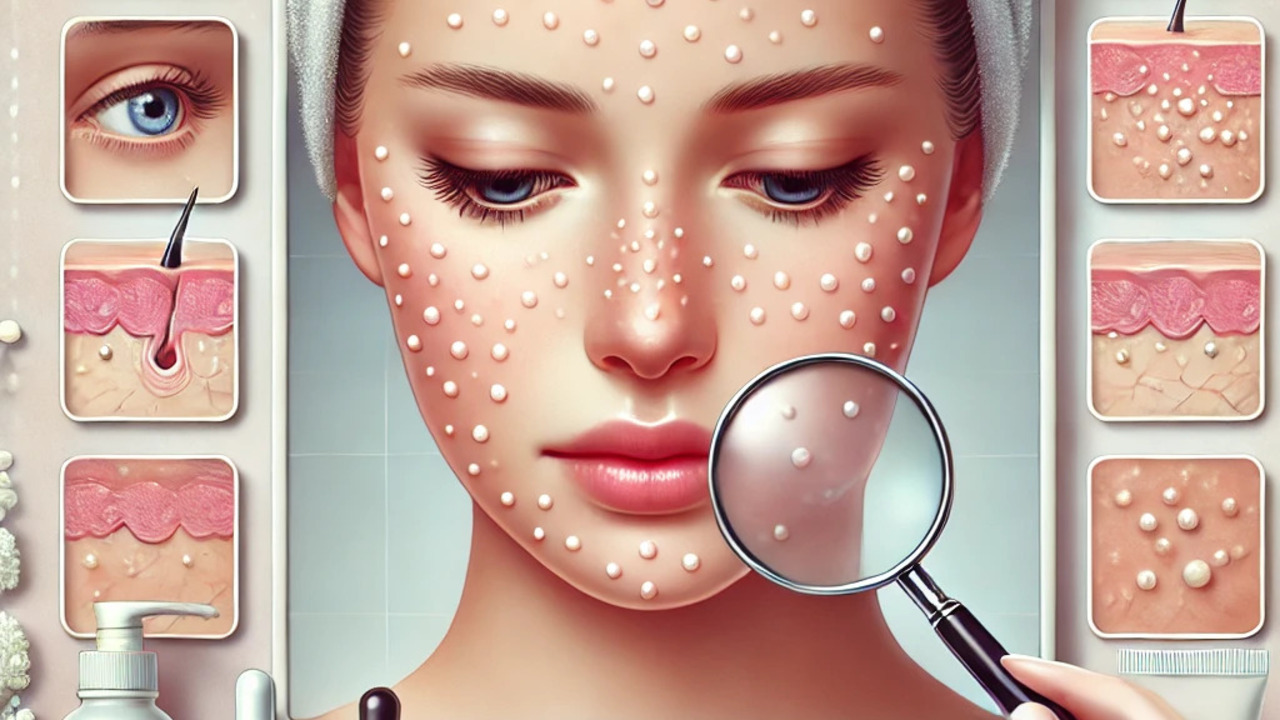
Milialar, a condition marked by tiny, white bumps on the skin, particularly around the eyes, cheeks, nose, and forehead, often raises concerns for those who encounter it. These bumps, also known as milia cysts, are composed of keratin, a protein that is a key component of the skin. Despite their harmless nature, they can be a source of cosmetic discomfort for many individuals.
Causes of Milialar
Keratin Overproduction and Entrapment
The primary cause of Milialar is the overproduction or entrapment of keratin. This protein, essential for skin protection, can sometimes become trapped beneath the surface, forming the characteristic white bumps. Hormonal imbalances, such as those experienced during puberty or menopause, can trigger this condition by disrupting the natural shedding process of the skin.
External Factors
Several external factors can also contribute to the development of Milialar. Prolonged exposure to the sun, especially without adequate protection, can damage the skin and exacerbate the formation of these bumps. Additionally, using heavy skincare products that clog pores and poor skincare hygiene can prevent the normal turnover of skin cells, leading to Milialar.
Symptoms of Milialar
Identifying Milialar
Milialar typically presents as small, white or yellowish bumps resembling sand grains. These cysts are common around the eyes, cheeks, nose, and forehead but can also appear on other body parts, such as the trunk or genitals. Although they are generally painless, some individuals may experience redness or irritation around the affected areas.
Misidentification
Due to its appearance, Milialar is often mistaken for other skin conditions like acne or warts. To avoid misidentification and ensure appropriate treatment, seeking medical advice for a proper diagnosis of Milialar is essential.
Diagnosis and Treatment
Professional Diagnosis
For a comprehensive understanding of Milialar, it’s important to highlight the role of dermatologists in diagnosing the condition. A physical examination is usually sufficient, but in some cases, a biopsy may be performed to examine a small sample of the affected skin under a microscope. This helps confirm the diagnosis and rule out other potential skin conditions, ensuring appropriate treatment and care.
Treatment Options
Treatment for Milialar depends on the severity of the condition. Professional extraction by a dermatologist using sterilized instruments is a common and highly effective method to remove the cysts safely. Chemical peels and microdermabrasion are other options that help exfoliate the skin and promote cell turnover, reducing the appearance of Milialar. These treatments offer hope and confidence in managing the condition.
Preventing Milialar
Skincare Routine
Maintaining a proper skincare routine is crucial in preventing Milialar. This includes using a gentle cleanser suitable for your skin type and avoiding heavy or comedogenic products that can clog pores. Regular exfoliation helps remove dead skin cells, reducing the risk of Milialar development.
Sun Protection
Protecting the skin from excessive sun exposure is also vital. Using sunscreen with a high SPF and wearing protective clothing can prevent sun damage, which can contribute to the formation of these cysts.
Lifestyle Changes
Addressing underlying causes, such as hormonal imbalances, through lifestyle changes or medical intervention can also help manage and prevent Milialar. Avoiding the temptation to self-remove the cysts to prevent infection and scarring.
Living with Milialar
Coping Strategies
Living with Milialar can be challenging, but several coping strategies and support resources are available. Educating oneself about the condition, its causes, and treatments can help individuals make informed decisions about their skincare routines and overall health.
Emotional Support
Emotional support from loved ones or online communities can also be beneficial. Sharing experiences and advice with others facing similar issues can provide comfort and practical tips for managing the condition.
Conclusion
Understanding the causes, symptoms, and treatment options for Milialar is crucial for effective management. By maintaining a proper skincare routine, protecting the skin from sun damage, and seeking professional medical advice, individuals can prevent and treat Milialar, ensuring healthier and clearer skin.
FAQs About Milialar
What is Milialar?
Milialar is a skin condition characterized by small, white or yellowish bumps, typically around the eyes, cheeks, nose, and forehead. These bumps, known as milia cysts, are filled with keratin and are generally harmless but can be a cosmetic concern.
What causes Milialar?
Milialar is primarily caused by the overproduction or entrapment of keratin beneath the skin’s surface. Factors such as hormonal imbalances, excessive sun exposure, heavy skincare products, and poor skincare hygiene can contribute to the development of Milialar.
How can I prevent Milialar?
To prevent Milialar, maintain a proper skincare routine by using a gentle cleanser, avoiding heavy or comedogenic products, and regularly exfoliating to remove dead skin cells. Protect your skin from excessive sun exposure using sunscreen and protective clothing. Addressing underlying hormonal imbalances can also help.
What are the symptoms of Milialar?
Milialar presents as small, white or yellowish bumps resembling sand grains. These cysts are usually found around the eyes, cheeks, nose, and forehead but can also appear on other body parts. They are generally painless but can cause redness or irritation in some individuals.
How is Milialar diagnosed?
A dermatologist can diagnose Milialar through a physical examination. In some cases, a biopsy may be performed to examine a small sample of the affected skin under a microscope, confirming the diagnosis and ruling out other skin conditions.
What treatment options are available for Milialar?
Treatment options for Milialar include professional extraction by a dermatologist, chemical peels, and microdermabrasion. Over-the-counter creams containing retinol or salicylic acid can help in mild cases. Prescription medications like topical retinoids or oral isotretinoin may be required for more severe cases.
Can I remove Milialar at home?
It is not recommended to remove Milialar at home as it can lead to infection and scarring. Professional extraction by a dermatologist using sterilized instruments is the safest and most effective method.
Is Milialar harmful?
Milialar is generally harmless and painless. While it can be a cosmetic concern for many individuals, it is important to remember that it does not pose a significant health risk. Seeking medical advice if there is any doubt or if the bumps are causing discomfort can help alleviate any anxiety.
Can Milialar reoccur after treatment?
Milialar can reoccur after treatment, especially if the underlying causes are not addressed. Maintaining a proper skincare routine and protecting the skin from sun damage can help prevent recurrence.
How long does it take for Milialar to go away?
The duration for Milialar to go away can vary depending on the treatment method and the individual’s skin condition. Professional treatments like chemical peels and microdermabrasion can speed up the process, while untreated Milialar may persist for months.
Are there any lifestyle changes that can help manage Milialar?
Addressing hormonal imbalances through lifestyle changes, such as a healthy diet and regular exercise, can help manage Milialar. Avoiding heavy skincare products and protecting the skin from sun exposure are crucial steps.
Is Milialar the same as acne?
No, Milialar is not the same as acne. While both conditions involve small bumps on the skin, Milialar consists of keratin-filled cysts, whereas blocked hair follicles typically cause acne and involve inflammation and bacterial infection.
Can children develop Milialar?
Yes, children can develop Milialar, especially newborns. It often appears on the face in infants and usually resolves independently without treatment.
Is Milialar contagious?
No, Milialar is not contagious. It cannot be spread from person to person through contact.
Also Read: Understanding Andrigolitis: Symptoms, Causes, and Management